Prashikshak Haryana
Site blog
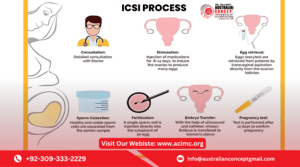
Intracytoplasmic Sperm Injection (ICSI) is one of the most advanced fertility treatment available today. It is a specialized form of In Vitro Fertilization (IVF) that involves injecting a single sperm directly into a mature egg to achieve fertilization. ICSI has become a breakthrough solution for couples dealing with male infertility and other specific reproductive challenges.
What Is the ICSI Procedure?
ICSI (Intracytoplasmic Sperm Injection) is typically performed as part of an IVF cycle. After the female partner’s eggs are retrieved, a skilled embryologist selects a single healthy sperm and injects it directly into each egg using a fine needle under a microscope. This technique helps overcome fertilization barriers that may not be addressed by conventional IVF.
Suitable Candidates for the ICSI Procedure
ICSI is not necessary for every couple undergoing IVF. It is specifically recommended in the following cases:
1. Severe Male Factor Infertility
ICSI was originally developed to treat male infertility. It is the first-line treatment when:
-
Sperm count is extremely low (oligospermia)
-
Sperm motility is poor (asthenozoospermia)
-
Sperm morphology is abnormal (teratozoospermia)
-
Sperm retrieved through surgical methods like TESE (Testicular Sperm Extraction) or micro-TESE
-
Ejaculation issues, including retrograde ejaculation or spinal cord injuries
In these cases, sperm may not be able to penetrate the egg on its own, making ICSI a suitable solution.
2. Unexplained Infertility
Some couples face infertility with no identifiable cause even after extensive testing. If standard IVF cycles fail, ICSI can be recommended as a next step to improve fertilization chances.
3. Previous IVF Failures
Couples who have undergone one or more unsuccessful IVF cycles due to failed fertilization may be advised to switch to ICSI. In such cases, even when sperm count and motility appear normal, there may be issues with sperm-egg interaction that ICSI can overcome.
4. Low Egg Yield or Quality
If the female partner produces a low number of eggs or the eggs retrieved are of poor quality, ICSI is often preferred to increase the chances of fertilization with each egg.
5. Use of Preimplantation Genetic Testing (PGT)
When couples opt for genetic testing of embryos (PGT-A or PGT-M), fertilization must be carefully controlled to avoid contamination. ICSI ensures that only one sperm fertilizes the egg, reducing the risk of inaccurate genetic results.
6. Fertility Preservation Cases
In cases where sperm or eggs are frozen before cancer treatments or surgery, ICSI improves the chances of fertilization when these preserved cells are later used.
When ICSI May Not Be Necessary
Not all IVF patients require ICSI. If both partners have normal fertility test results, good egg count, and healthy sperm parameters, conventional IVF might be sufficient. Overuse of ICSI in such cases may add cost without providing additional benefit.
Final Thoughts
ICSI has transformed the landscape of fertility treatment, especially for couples facing male infertility and failed fertilization. If you're struggling to conceive and fall under any of the categories mentioned above, you may be a suitable candidate for the ICSI procedure.
However, the decision should always be made with guidance from a qualified fertility specialist, who will evaluate your specific medical history, test results, and previous treatment outcomes to recommend the best approach.